Abstract
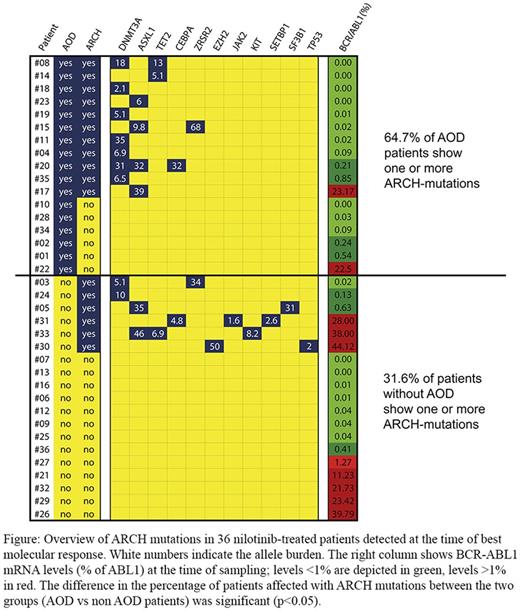
Although otherwise considered a relatively safe drug, the BCR/ABL1 tyrosine kinase inhibitor nilotinib has recently been associated with the occurrence of progressive arterial occlusive disease (AOD). In most of the affected patients, cardiovascular risk factors have been identified. However, AOD may even occur in patients without known risk factors. The aim of this project was to identify clinical and molecular risk factors predicting AOD development in CML patients receiving nilotinib. A total number of 36 consecutive nilotinib-treated patients with Ph+ CML (median age: 49 years; m/f ratio: 1.25, all seen at our department between 2006-2013) were examined. With the exception of one case, none of these patients had developed an AOD before nilotinib-therapy. During nilotinib therapy, AOD events were found to accumulate over time. After 2.0 years, 29.4% of our patients had developed one or more AOD events. After 3.0 years, the frequency of AOD increased to 38.9%, and after 3.7 years, it reached 47.2%. After 3.7 years, a total number of 39 symptomatic AOD events were recorded, resulting in 32 AOD-events per 100 patient-years and a 1-year hazard ratio of 4.72 compared to the AOD-risk of healthy individuals (p<0.01). No venous thromboembolic events were recorded. The frequency of patients with severe AOD did not further increase after 3.0 years which may be due to better patient-selection, drug-discontinuation, and co-medication consisting of aspirin, statins (hypercholesterolemia) and anti-diabetic drugs (diabetes mellitus). In a first step, we applied the European Society of Cardiology (ESC) SCORE. A substantial number of our patients were at high risk for AOD-development according to this score (ESC-SCORE ≥5: 5/36=13.9%). As expected we found a positive correlation between a high ESC-SCORE (≥5) and the development of AOD (AOD+: 4/5 patients; AOD-: 1/5 patients). In an attempt to identify additional risk factors, molecular and serologic studies were performed. First, we screened for well-established classical molecular risk factors. In these studies, no Factor-V Leiden- and no prothrombin mutations were detected. The median levels of protein C and protein S were found to be lower in patients with AOD compared to those without AOD (protein C, AOD: 103% vs non-AOD: 132%; protein S, AOD: 67% vs non-AOD: 105%). We also detected a correlation between the blood group status and the occurrence of AOD: non-0 status in AOD patients: 73.3% vs non-0 status in non-AOD patients: 52.9%. Next we examined our patients for the presence of age-related somatic mutations (ARCH) as recent data have shown that such mutations (in TET2, ASXL1, DNMT3A, ZRSR2, CEBPA, and SF3B1) are associated with an increased risk of healthy individuals to develop a myeloid neoplasm but also to develop a severe cardiovascular disease (Jaiswal et al, N Engl J Med 2014;371:2488-2498). In our study, we found that these ARCH mutations, especially mutations in TET2, ASXL1, and DNMT3A, are more frequently detected in CML patients who developed AOD during nilotinib-treatment compared to those who did not develop AOD (AOD in mutation-positive patients: 11/17=65% vsAOD in mutation-negative patients: 6/19=32%, p<0.05) (Figure). These mutations were detected at the time of partial or complete molecular response but also in patients with residual CML (BCR-ABL1 mRNA >1%-44%). The allele burden of age-related mutations ranged between 2% and 68%. In one patient without AOD, low levels (1.6% allele-frequency) of JAK2 V617F were detected. In conclusion, multiple clinical and molecular risk factors predict the occurrence of AOD development in nilotinib-treated patients with CML. Based on our results the major recommended tool for prognostication is the ESC-SCORE. However, additional factors, like protein C and S, the blood group and age related mutations detected by NGS after debulking of the dominant BCR-ABL1+ sub-clones, should also be taken into account. Together with optimal metabolic control and co-medication, these recommendations may lead to optimal patient-selection and better control and management of vascular side-effects in nilotinib-treated patients with CML.
Hadzijusufovic: Novartis: Honoraria. Hoermann: Gilead: Honoraria, Research Funding; Ariad: Honoraria; Novartis: Honoraria; Amgen: Honoraria. Sperr: Amgen: Consultancy, Honoraria, Research Funding; Meda: Research Funding; Celgene: Consultancy, Honoraria; Phadia: Research Funding; Teva: Honoraria; Novartis: Other: Register. Jilma: Biomed: Research Funding; Arsanis: Research Funding; Baxalta: Research Funding; Emcools: Research Funding; Bayer: Research Funding; Syntheract: Research Funding; Valneva: Research Funding; Boehringer Ingelheim: Research Funding; TrueNorth Therapeutics Inc.: Consultancy; Octapharma: Research Funding; Prediction Biosciences: Research Funding; Recardio: Research Funding; Themis: Research Funding; TrueNorth Therapeutics: Research Funding; Bioverativ: Research Funding; JHL: Research Funding; VitaerisBios: Research Funding. Schernthaner: Amgen: Honoraria; Astra Zeneca: Honoraria; Boehringer Ingelheim: Honoraria; BMS: Honoraria; Elli Lilly: Honoraria; Merck: Honoraria; Novo-Nordisk: Honoraria; Novartis: Honoraria; Pfizer: Honoraria; Sanofi-Aventis: Honoraria. Valent: Teva: Honoraria; Ariad: Honoraria, Research Funding; BMS: Honoraria; Incyte: Honoraria; Novartis: Honoraria, Research Funding; Blueprint: Research Funding; Pfizer: Honoraria; Deciphera: Honoraria, Research Funding; Celgene: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal